What Is IBS?
Have you been told you have irritable bowel syndrome (IBS) and that left you wondering what caused it and what you can do about it?
Since IBS is a functional disorder of the gut-brain interaction, there is no diagnostic test for it or even single treatment for it.
While this can be disappointing to hear, there are clear drivers at place with IBS that can explain why symptoms are present and give you guidance on how to address those. In this article, I’ll cover how IBS is diagnosed, what causes it, and what drivers are at play you can address.
How is IBS diagnosed?
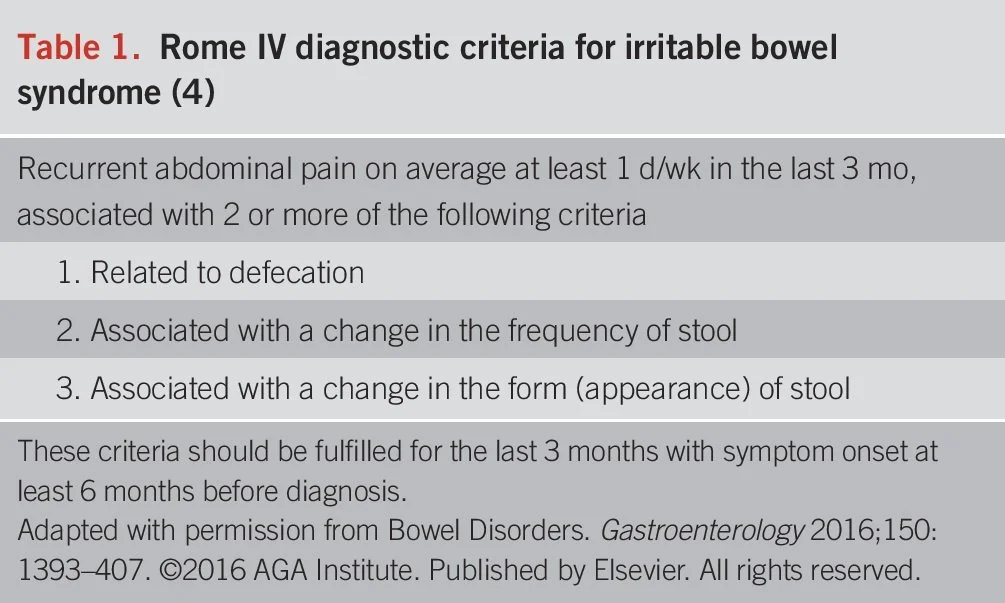
IBS is diagnosed based on symptoms and the duration of those symptoms, according to the Rome IV criteria, which you can see pictured below. This means that a diagnosis of IBS must involve changes in motility, or movement of stool through the gastrointestinal (GI) tract, and pain.
Typically, other conditions will be screened for or ruled out before an IBS diagnosis is made. This includes blood tests to screen for celiac disease and inflammatory bowel disease (IBD). There is not a standard diagnostic process for IBS, so each provider may screen or test for different conditions according to their own practice.
To get the best screening and diagnosis possible, communicate all of your symptoms and your health history in as concise as a manner as you can, and maintain care with your gastroenterologist as you work on your condition so that any red flags can be addressed.
Source: Official journal of the American College of Gastroenterology | ACG116(1):17-44, January 2021.
What are common IBS symptoms?
Common symptoms with IBS include gas, bloating, pain, and constipation and/or diarrhea.
There are different types of IBS and when you get diagnosed, you may get a designation at the end of your diagnosis, but you may not. Not everyone uses these and these can change, but in general, we do have these four types that are used:
IBS-C is constipation predominant, so that means most of the time you present with constipation.
IBS-D stands for diarrhea predominant, so that means most of the time you present with diarrhea.
IBS-M would be mixed. this means you have a cycle of constipation and diarrhea.
IBS-U for unspecified. This one is not as commonly used, but it does exist.
What causes IBS?
Potential causes of IBS include chronic antibiotic use, foodborne illness or viral infections, chronic stress, and other factors that change the microbiome (cancer treatment, surgery, etc).
Most people develop IBS symptoms long before a diagnosis is made, so it can be tough to pinpoint the exact cause. Many times, IBS symptoms will show up in times of stress, like during college, in pregnancy, or with the start of a new job or transition. This doesn’t mean the stress caused IBS, but likely means this was a trigger for symptoms to turn on after IBS was already present. This is all still not well known.
Currently, there are no known negative health risks associated with IBS. However, quality of life surveys show that IBS has a massive negative effect on a person’s quality of life, which can increase risk for depression and mood disorders, as well as eating disorders. Due to restriction of food groups seen among those with IBS, malnutrition and nutrient deficiencies are also a concern.
Foodborne Illness
Foodborne illness is the most well understood cause of IBS, thanks to recent research in this area. When the body is infected with pathological bacteria, Campylobacter species most common in the case for IBS, these bacteria produce the toxin CdtB. This can happen over a few weeks after initial infection.
Over a couple of months, the body produces antibodies to fight CdtB and a protein found in CdtB called vinculin. These are called anti-CdtB and anti-vinculin antibodies. Anti-vinculin antibodies get into tissues and can cause nerve damage and autoimmune reactions, including in the gut, and anti-CdtB antibodies are associated with dysbiotic microbiota profile (covered more below).
Over time, the shifts in the body from these antibodies will then start to produce IBS symptoms. These are also believed to be the main cause of visceral hypersensitivity, which is seen with IBS. This is where sensations in the GI tract are communicated to the brain and then the brain sends increased pain signals, leaving the personal experiencing the sensation in significant pain that others would not experience from the same sensation.
There is some thought that this could lead to altered immune reactions, which could classify some of IBS as an autoimmune condition in the future. There’s a lot that still needs to be researched here.
We refer to IBS that has been caused by foodborne illness as post-infectious IBS (PI-IBS). There is actually a test to look at these antibodies and confirm this caused, called the IBS Smart Test. You can ask your doctor about this if you are curious.
We also see a similar effect happen post viral infections, including COVID. After the pandemic of 2020, we are seeing a rise in post-COVID IBS, which means other viral infections could be causes to evaluate in your history
Want to learn more about IBS? Sign up for a free IBS mini course here!
drivers of ibs
When you get IBS, there are 4 major “drivers” of the condition that are responsible for the change in gut function and the susceptibility to symptoms. These drivers are:
Dysbiosis
Altered motility
Gut-brain miscommunication
Altered immune activation
Dysbiosis
The gut is made up of over 100 trillion microorganisms, including bacteria, viruses, phages, yeast, and fungi. This is over 10x the number of human cells in the body! This collection of organisms is referred to as the gut microbiota. The gut microbiome refers to the microbes and all of their genetic material, which contains over 3.3 million genes.
With IBS, the makeup of bacteria, or microbiome, is not ideal, which we refer to as dysbiosis. That means there aren’t as many beneficial bacteria present, and there may be an increase in not so great or pathogenic gut bacteria. With current research, we see around 50% of those with IBS have what’s called a pathogenic microbiome profile, compared to a healthy profile in the other 50%.
The dysbiosis may be caused by foodborne illness (mentioned in the section before), overuse of antibiotics, chronic stress, treatments that disrupt the gut, and diet/lifestyle behaviors. The exact reason for this profile in IBS is likely linked back to the foodborne illness piece, but this still needs to be explored more.
Altered motility
Gut motility refers to the movement of the muscles that makeup the GI tract. Changes in motility means that these muscles either move too quickly (hypermotility) which can cause diarrhea, or they move too slowly (hypomotility) which can cause constipation. This can be related to, or independent of, the other dirvers.
Gut-brain miscommunication
Your gut and brain are connected through the HPA axis, which is really a connection between two nervous systems - the central and enteric nervous systems. Through this communication, each nervous system can impact the other.
With IBS, the communication pathway is off, which can lead to a disconnect in gut function, a rise in pain with gut sensations, and an impact on mood in addition to what’s going on in the gut.
Altered immune activation
The majority of your immune cells are in your gut. Your gut itself provides a barrier from what you take in from the world and in the inside of your body. As I mentioned earlier in the cause of post infectious IBS, some with IBS have altered immune reactions to things they shouldn’t.
This can impact pain sensitivity, gut function, food tolerance, and the balance of microbes in the gut.
What This Means for You
It’s true that there’s a lot we still don’t understand about IBS, which may leave you feeling discouraged and confused. The good news is that a lot of research has been done and there’s still so much more coming.
No matter the cause, it’s helpful to know that there are different layers to IBS and different ways we can address those. That’s something our team of dietitians at Gutivate assess for and focus on in our care plans with clients. If you’re looking for that level of individual care and are interested in what we do at Gutivate, you can start by scheduling a consult call here.
Do you want clear guidance to manage your IBS so you can feel confident in your body again?
Guides: